Clinical takeaway (TL;DR): A meaningful proportion of patients clinically diagnosed with Alzheimer’s disease (AD) also harbor α-synuclein (Lewy-type) pathology, in addition to the well-characterized amyloid-β (Aβ) plaques and tau neurofibrillary tangles. This trio is associated with faster progression and different symptom profiles (for example, visual hallucinations and behavioral disturbances), which should shape prognosis and treatment decisions.1
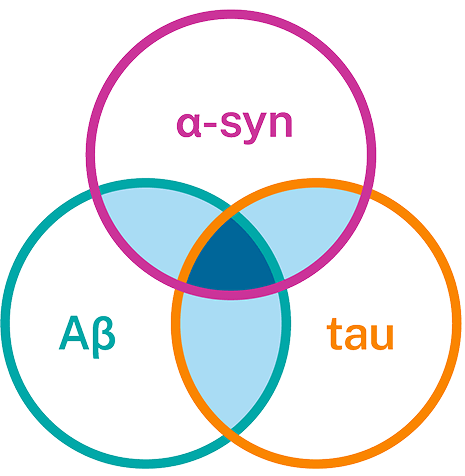
The reality: mixed tau–amyloid–α-synuclein pathology is common
Neuropathology and modern biomarker studies converge on the finding that AD frequently coexists with Lewy-type (α-synuclein) pathology. Autopsy studies report substantial overlap: many autopsy series report 40–60% of AD patients harbor Lewy-type synucleinopathy, and molecular biomarker studies detect α-synuclein pathology in about 30% of living patients clinically diagnosed with AD.1 However, reported rates vary by cohort and method (neuropathology vs CSF seed amplification assay).1 Why the range? Differences in ascertainment (clinic vs community), demographics, and the sensitivity of detection methods (immunohistochemistry vs seed amplification assays) all affect prevalence estimates. These estimates are consistent among clinical and neuropathological cohorts.1

Mixed pathology changes the clinical picture — what to watch for
Clinically, the addition of α-synuclein (α-syn) pathology is not silent:
- Patients with coexisting α-syn often show earlier and more rapid cognitive decline and more prominent visuospatial dysfunction, fluctuations, and neuropsychiatric symptoms than “pure” AD.1,2
- Multiple large clinicopathologic studies and cohort analyses link mixed pathology to shorter time from symptom onset to dementia progression and higher mortality.3
Takeaway: if an AD patient presents with well-formed visual hallucinations, marked fluctuations, parkinsonism, and/or disproportionate visuospatial impairment, consider testing for co-existing Lewy-type pathology. Understanding the underlying biology will allow for relevant counseling and precise management.1,2
Detecting the trio in vivo: biomarkers and imaging that help
We now have tools that increase our ability to detect mixed pathology before autopsy:
- CSF α-syn seed amplification assay (αS-SAA): recent studies show αS-SAA can identify α-synuclein co-pathology in clinically diagnosed AD patients, and that SAA positivity correlates with particular clinical features (e.g., visuospatial impairment) and worse outcomes.1
- CSF and plasma Aβ/tau assays and amyloid/tau PET remain the backbone for identifying AD-type pathology (Aβ and tau). Combining these AD biomarkers with αS-SAA results and/or with clinical signs increases confidence in recognizing mixed disease.4
- Multimodal approaches (clinical symptoms, fluid biomarkers, PET) are the most informative for identifying overlapping pathologies in vivo. Emerging work links α-syn co-pathology with accelerated tau accumulation detectable by serial biomarkers, underscoring that these pathologies interact dynamically.5
Practical note: αS-SAA testing is available in research and in the clinic; when ordered, it provides complementary information to Aβ/tau testing and should be considered when the clinical picture is atypical or for prognostic clarification.1
Mechanisms — how α-syn, tau, and Aβ interact
Preclinical and human pathology data indicate cross-talk among these proteins:
- α-Syn can promote tau hyperphosphorylation and aggregation; conversely, Aβ and APOE genotype may modulate α-syn pathology. Experimental mouse models and human tissue studies support a bidirectional interaction that can accelerate neurodegeneration when these proteins co-aggregate.6
- Recent longitudinal biomarker work suggests that α-synuclein co-pathology is associated with faster amyloid-driven tau accumulation, offering a plausible mechanism for the observed clinical acceleration in mixed pathology cases.5
Implication: coexistence is more than “two diseases in one brain”—protein interactions may aggravate pathology and clinical decline.6
What this means for disease management
For clinicians managing patients with suspected or confirmed AD, recognizing possible tau–Aβ–α-syn mixed pathology has practical implications:
- Prognosis & counseling: Expect potentially faster progression and higher likelihood of neuropsychiatric features in patients with mixed pathology; discuss this sensitively with patients and families.1,2
- Medication choices: Coexisting Lewy-type pathology may increase sensitivity to neuroleptics and influence treatment of parkinsonism and psychosis; be cautious with certain antipsychotics (e.g., Haldol) and consider the lowest-effective doses and nonpharmacologic strategies where possible. (Clinical judgement based on phenotype remains essential.)2
- Disease-modifying therapies: Mixed proteinopathy may affect therapeutic response. Consider α-syn SAA CSF biomarker testing to prevent confounding variables in treatment decisions.7
Quick practical checklist for recognizing the trio in the clinic
- Red flags suggesting α-syn co-pathology in an AD patient include: early/marked visuospatial impairment, visual hallucinations, parkinsonism, cognitive fluctuations, extrapyramidal signs, REM sleep behavior disorder.1,2
- Tests to consider when mixed pathology is suspected: CSF or plasma Aβ/tau panel, amyloid/tau PET if available, and α-syn SAA; document and monitor symptom trajectory closely.4
- Use results to inform prognosis, safety counseling (medication sensitivity), and caregiver planning.2,5

Bottom line
Mixed proteinopathy that specifically includes tau, amyloid-β, and α-synuclein is common and clinically meaningful in Alzheimer’s disease. Recognizing it matters for prognosis, symptomatic management, and counseling. Use clinical red flags and multimodal biomarkers (Aβ/tau assays + α-synuclein SAA) to stratify patients and tailor care. Continued adoption of sensitive assays and inclusion of mixed pathology stratification in research will sharpen our ability to personalize therapy for these patients.1
- Alzheimers Dement. 2024 Feb 7;20(4):2444–2452. doi: 10.1002/alz.13658
- Alzheimers Dement.2021 May 18;13(1):e12189. doi: 10.1002/dad2.12189.
- J Alzheimers Dis Parkinsonism.2018;8(4):444.doi: 10.4172/2161-0460.1000444.
- Alzheimers Dement. 2024 Jun 21;20(8):5757–5770. doi:10.1002/alz.14039
- Mol Neurodegener. 2025 Mar 18;20:31. doi:10.1186/s13024-025-00822-3
- Mol Neurodegener. 2019 Jun 11;14:23. doi:10.1186/s13024-019-0320-x
- J Alzheimers Dis Parkinsonism. 2018 Aug 10;8(4):444. doi:10.4172/2161-0460.1000444
Get in the Know
Bring biological certainty to your diagnosis with Amprion's SAAmplify-ɑSYN test. Order your shipping kits today and help move your patient beyond a probable diagnosis.